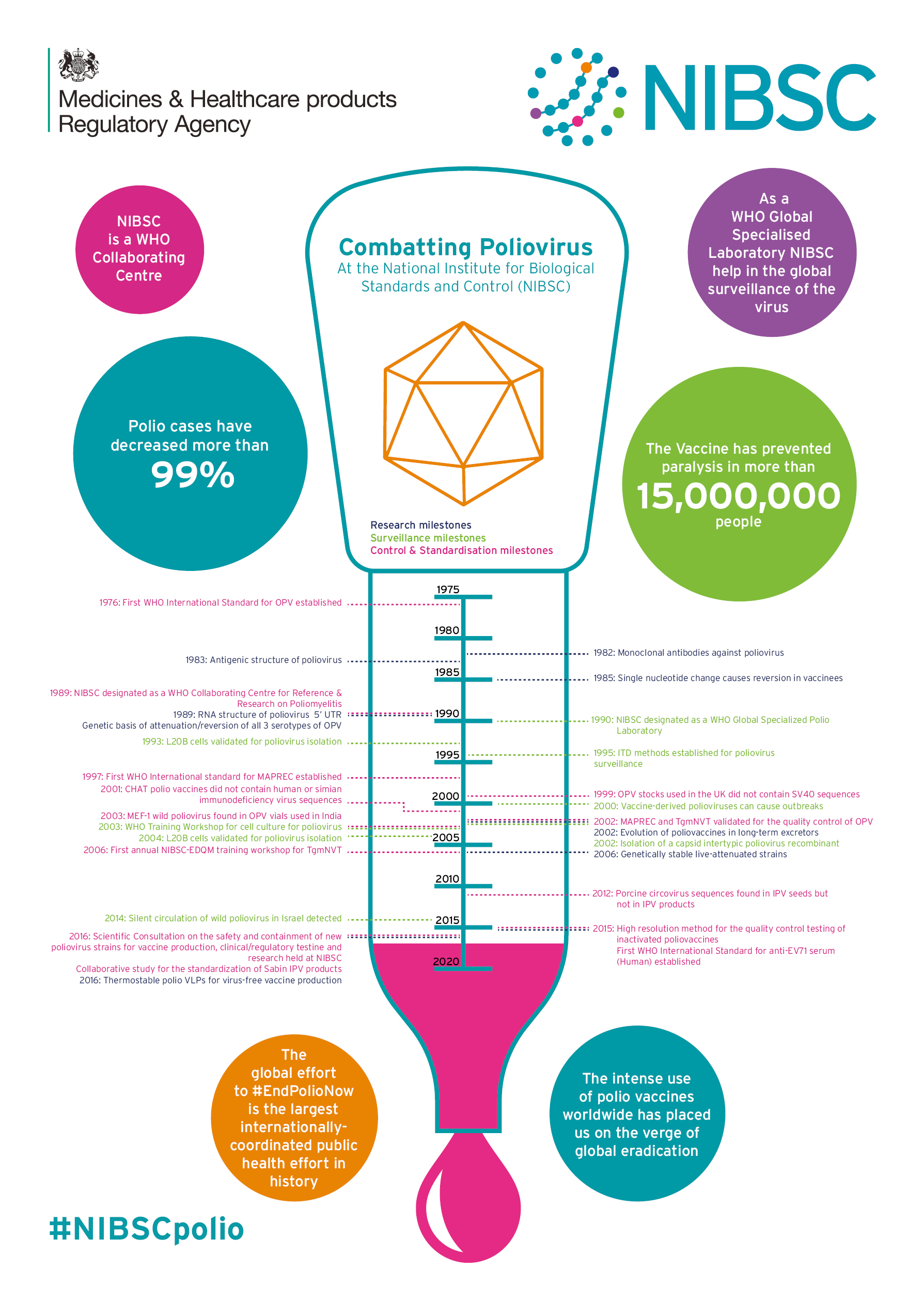
How research at NIBSC is helping in the final push to eradicate polio
The world has made tremendous progress toward the eradication of polio. In 1988, wild poliovirus was present in more than 125 countries and paralysed 350,000 people every year, primarily young children. Vital research at NIBSC is helping to ensure that polio becomes a disease of the past.
During the 1940’s and early 1950’s, polio was the disease dreaded by every parent, just as meningitis is today. Healthy children were struck down, paralysed and confined to “iron lungs” after seemingly harmless activities such as going to the swimming pool. In the USA, a campaign to eliminate paralytic polio was championed by President Roosevelt - himself a sufferer - and driven by charitable donations including “The March of Dimes”. This resulted in the development of two vaccines in the mid 1950’s, hailed as medical breakthroughs, which turned the tide against this terrible disease.
Today, the intense use of polio vaccines worldwide has placed us on the verge of global eradication of polio. Ironically, the vaccines that have been instrumental in controlling polio could now be preventing us from achieving our goal. If we fail to eradicate this highly contagious disease, we could witness a resurgence of as many as 200,000 new cases annually.
Here, we describe how NIBSC continues to play a leading role in the final push for eradication.
The first vaccines
The global workhorse in polio eradication has been the live, but weakened “Sabin” vaccine which is given either on a sugar lump or by squirting the salty vaccine into the mouth. It works by infecting cells in the gut which then generate immunity. Crucially, the vaccine cannot invade the central nervous system and cause the hallmark paralysis of the virulent virus. Research at NIBSC carried out 30 years ago uncovered a dark secret about this “harmless” vaccine. By looking at the genetic sequence of virus excreted into the nappies of babies after vaccination, the NIBSC team showed that within a couple of weeks, the weakened vaccine reverts to a form able to cause disease again. This risk is not just a theoretical conjecture. In virtually every part of the world, apart from Pakistan and Afghanistan, reported outbreaks of paralytic polio arise from infection of unvaccinated people with reverted Vaccine Derived Polio Viruses (VDPV). The weakened vaccine is both cheap to produce, and safe and easy to deliver as syringes and needles aren’t needed, but its ability to revert is a major weakness in the eradication programme. This important discovery helped shape the subsequent global programme of polio eradication.
The search for alternative vaccines
The alternative polio vaccine that is increasingly used, particularly in Europe and North America, is the inactivated “Salk” vaccine which involves growing vast tanks of virus and then inactivating it with chemicals to produce the vaccine. The advantage is that the virus is dead so it cannot revert (although a syringe and needle are required to inject it). The challenge is how to produce huge vats of virulent virus in a world where the virus has largely been eradicated. The risk is significant, especially if the virus escaped and got into drains where it could survive for a long time. At NIBSC, we are working to find solutions to overcome this challenge.
NIBSC as a WHO Collaborating Centre
NIBSC is a WHO Collaborating Centre for Reference and Research on Poliomyelitis which involves sending our expert scientists all over the world to advise vaccine manufacturers. An increasing number of companies want to produce inactivated polio vaccine to meet the increased demand for the “safer” existing vaccine; our experts help ensure that new manufacturers produce high quality vaccines. New and established vaccine producers are now considering whether they can produce an effective and safer inactivated vaccine from growing the weakened Sabin strains and inactivating it. There are, however, concerns that the inactivated Sabin vaccine is not as effective in stimulating the specific anti-polio antibodies (against the D antigen) that protect against paralytic polio. Work by NIBSC to produce physical standards used as references in measuring the D antigen content of these vaccines and the specific antibodies in the serum of vaccinated individuals is critical to establishing the effectiveness of these inactivated Sabin vaccines.
NIBSC is one of seven WHO Global Specialised Polio Laboratories advising scientists in a global network of regional and national diagnostic laboratories that investigate every case of acute flaccid paralysis and decide whether polio infection is involved. Our experts also undertake routine surveillance of sewage for evidence of poliovirus. For example, Israel has a high level of polio vaccination with the inactivated Salk vaccine and has had no recorded cases of polio disease for some years. Worryingly though, wild-type polio was detected in their sewage samples in 2013/2014. So how can disease causing polio get into sewers? It had been shown that the virus was imported from Pakistan - one of two remaining countries endemic for polio. Working with colleagues in Israel, NIBSC analysed the properties of virus isolates from samples taken from Israeli sewers and established how current vaccines protect against them. We discovered that whilst high levels of vaccination can prevent cases of wild-type polio occurring, the absence of disease does not necessarily lead to an absence of virulent virus circulating in a population that has been immunised with inactivated vaccine. This key finding informed vaccine policymakers who then decided to re-introduce the Sabin vaccine in Israel. This serves as a warning that we must be extremely cautious about stopping polio vaccination, even in countries where there have been no cases of disease for many years.
An evolving vaccine and genetic susceptibility – a perfect storm for polio
The NIBSC team has highlighted another major concern that will shape the end strategy of the global polio eradication. As part of a study in 1995 of gastro-intestinal infections amongst hypo-gammaglobulinaemic patients with inherited disease (common variable immunodeficiency) that results in them producing only poor antibody responses following infection, one patient was found to be excreting culturable poliovirus. The patient was not diagnosed at birth and was given the live weakened Sabin vaccine. Since 1995, the NIBSC team has detected the poliovirus in every stool sample collected from that patient, and so the evolution of the virus over more than 20 years has been defined. This has shown that the virus is fully capable of causing disease. Once again, these data show that vaccination against poliovirus, maintaining surveillance activities and developing anti-viral therapies to cure these patients may be necessary for many decades to come.
NIBSC vaccine research continues
Is it possible to break out of this complex web of continuous vaccination? The development of weakened strains of poliovirus that cannot revert to virulent forms would be one valuable step which would make dealing with situations like the one in Israel less hazardous because the vaccine itself couldn’t cause disease if it spread to unvaccinated areas. Other possibilities include developing an inactivated vaccine disabled in ways that would prevent it escaping from vaccine plants; creating synthetic vaccines that don’t carry the viral nucleic acid would mean they cannot infect people. All of these ideas are being investigated by the team at NIBSC. So far, we have designed a weakened Sabin-like vaccine which appears unable regain virulence like the current Sabin vaccine. This is ready to test in humans within the next year.
Producing large amounts of poliovirus in order to prepare the inactivated Salk vaccine would be much safer if the virus could only grow in tissue culture and not in people. This is precisely what a specially engineered strain called S19 is able to do. Careful molecular modification of part of the virus nucleic acid has locked in attenuating mutations which do just that. This novel vaccine virus has been taken up by a major vaccine manufacturer to investigate whether it can be scaled-up successfully. In an attempt to make an even safer poliovirus vaccine, the different proteins that make up the virus coat are being produced in cells in tissue culture in a way that enables them to spontaneously fold up together to make a virus particle, devoid of nucleic acid. The nature of these viral proteins makes this relatively straightforward. However, for native virus, unless viral nucleic acid is inside stabilising the structure, these particles will fall apart at just over 30°C. Working collaboratively with teams at the Universities of Reading, Oxford and Leeds, we have devised ways of engineering more stable “empty” virus particles, and the antibody responses generated by this next generation of “safe” vaccines are now being investigated.
At NIBSC, the valuable knowledge and expertise gained by studying existing vaccines continues to be translated into innovative safer new vaccines. The hope is that the Salk and Sabin vaccines will no longer be needed and, within a generation, polio will be gone - forever.