Pandemic influenza
For an influenza virus to cause a pandemic it has to be:
- new to humans so that there is little to no protective immunity in large parts of the population
- able to spread easily from human to human
A wide range of influenza A viruses are found in wild birds and domestic poultry. Most of these will not be recognised by the immunity in people who have had seasonal influenza or been vaccinated against it – and so they will be new to the human immune system.
Meanwhile it is hard to predict which viruses might transmit between humans.
In recent years, there have been cases of human infection with animal – particularly avian – viruses in different countries and regions. This includes avian A(H5N1) in a number of countries and A(H7N9) in China.
The pandemic of 2009 – caused by an A(H1N1) virus of swine origin – showed how rapidly a pandemic can spread around the world.
Vaccines are the best way to protect people from influenza and pandemic influenza. But developing a new pandemic vaccine takes time and vaccines may not be available for the first wave of a pandemic.
Preparing for a pandemic
There are several elements involved in preparing for a pandemic. A crucial one is preparing – ahead of time – candidate vaccine viruses (CVVs) for manufacturing vaccines against viruses that could cause a pandemic in the future.
Having CVVs available before a pandemic emerges means time can be saved in producing vaccines. Also with these CVVs we can gain valuable experience of various subtypes of influenza A – from evaluating growth and yield characteristics to developing trial batches of vaccine and assessing them in clinical trials.
We have been producing CVVs for potentially pandemic viruses for several years. We have also generated reference reagents for testing the potency of inactivated vaccines made from these CVVs.
Candidate vaccine viruses
CVVs for influenza A are usually reassortant viruses with the genes encoding the surface glycoproteins of haemagglutinin (HA) and neuraminidase (NA) derived from the wild-type (wt) virus of interest – such as an A(H5N1) virus – and most or all of the other six gene segments derived from a high-growth donor virus.
The high-growth donor virus, usually the strain A/Puerto Rico/8/34 (PR8), grows well in the substrate for vaccine production – usually embryonated chicken eggs – and confers high-growth properties to the resulting reassortant virus.
So-called classical or conventional high growth reassortants (HGRs) are produced via double infection of eggs with two viruses.
A different method is used for many viruses with pandemic potential – reverse genetics (RG) technology.
Reverse genetics (RG) for generating CVVs
We use eight plasmids – each encoding an entire RNA genomic segment – and four additional support plasmids that express the three subunits of the influenza A virus polymerase complex and the viral nucleoprotein.
We introduce these plasmids into cells in culture and initiate an infectious cycle, so producing infectious influenza viruses. RG allows us to alter viral genes by introducing targeted nucleotide changes into the RG plasmids.
We take advantage of this to attenuate CVVs derived from highly pathogenic avian influenza viruses of subtype H5 and H7. In these viruses, the main determinant for high pathogenicity in poultry is a multibasic protease cleavage site in the HA protein. We can remove this stretch of basic amino acids by deleting the corresponding nucleotides in the HA gene.
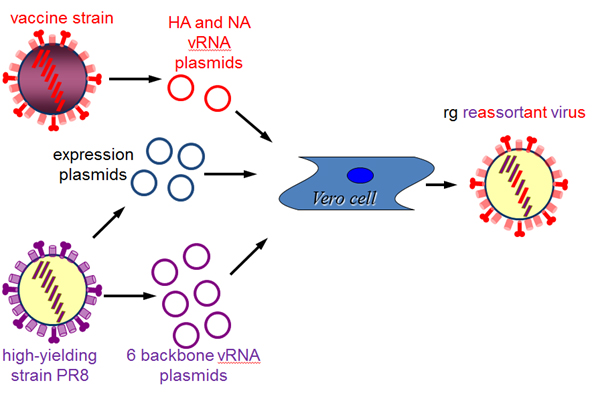
Schematic representation of the generation of a reassortant influenza virus by reverse genetics technology.
Using both RG technology and classical reassortment, we have generated a number of CVVs for viruses of pandemic potential. Our choice of viruses for developing CVVs is guided by a risk assessment of wild-type avian viruses that can infect humans and/or other mammals.
We are part of and work closely with the World Health Organisation (WHO) Global influenza surveillance and response system (GISRS). The GISRS regularly examines evidence from around the world about zoonotic influenza and characterises viruses of pandemic concern. It also recommends viruses for the development of new CVVs.
These candidate influenza vaccine viruses are developed at NIBSC using materials that are subject to third party rights. Therefore a Materials Transfer Agreement (MTA) may be required before we can supply these viruses. All recipients of the materials covered by an MTA must respect the rights of the owners of the plasmids on which NIBRG materials are based, and the reverse genetics engineering processes used to make these strains safe.
Characterisation of pathogenicity of (pre)pandemic CVVs
Producing vaccine involves propagating CVVs on a large scale so it is important that new CVVs can be handled safely in vaccine manufacturing facilities.
Wild-type (wt) viruses of high pathogenicity are generally unsuitable for vaccine production, and new CVVs generated from potentially pandemic and pathogenic wt viruses need to be attenuated relative to their wt parental virus. The WHO has issued guidance on how to test attenuation of CVVs.
The panel of tests used varies between different parental viruses, but usually includes assessing pathogenicity in the ferret model. We conduct safety tests of new CVVs according to WHO guidelines.
Reference reagents for (pre)pandemic CVVs
The potency of inactivated influenza vaccines is measured using the single radial immune diffusion test (SRD).
The test requires a calibrated antigen reference reagent and a specific antiserum reagent. NIBSC has produced reagents for a number of prepandemic CVVs. These are generated in a similar way to reagents for seasonal influenza viruses.
WHO Pandemic Influenza Preparedness (PIP) Framework
As a WHO Essential Regulatory Laboratory (ERL), we comply with the WHO Pandemic Influenza Preparedness (PIP) Framework.
We share all CVVs for viruses of pandemic potential with interested researchers and vaccine manufacturers under the conditions of the PIP Framework, specifically the SMTA2.
All shipments of viruses covered by the PIP Framework are entered into the WHO Influenza Virus Traceability Mechanism (IVTM) where details of shipments are public.
Available viruses and reagents
|
Virus
|
subtype
|
Candidate vaccine virus
|
Antigen reagent
|
Antiserum reagent
|
|
A/duck/Singapore/97
|
H5N1, clade 0
|
NIB-40
98/610
|
00/552
|
00/542
(Ck/Scot/59)
|
|
A/Hong Kong/213/2003
|
H5N1, clade 1
|
NIBRG-12a
08/154
|
|
00/542
(Ck/Scot/59)
07/148 2
09/192 1,2
|
|
A/Vietnam/1194/2004
|
H5N1, clade 1
|
NIBRG-14a
11/130
|
09/184
|
07/148 2
09/192 1,2
|
|
A/Cambodia/R0405050/2007
|
H5N1, clade 1.1
|
NIBRG-88a
13/176
|
08/216
|
08/210 2
|
|
A/turkey/Turkey/1/2005
|
H5N1, clade 2.2.1
|
NIBRG-23a
08/156
|
07/112
|
06/192
08/1263
|
|
A/Anhui/1/2005
|
H5N1, clade 2.3.4
|
Anhui/01/2005(H5N1)-PR8-IBCDC-RG5 (Virus available from CDC)
|
07/290
|
07/338
08/142 2
|
|
A/turkey/Italy/3889/1999
(low path)
|
H7N1
|
Wild type
12/122
|
|
02/294
|
|
A/mallard/Netherlands/12/2000
|
H7N3
|
NIBRG-60 a
07/204
|
07/336
|
07/2782
|
|
A/mallard/Netherlands/12/2000
|
H7N1
|
NIBRG-63 (7:1 reassortant) a
08/250
|
|
|
A/New York/107/2003
|
H7N2
|
NIBRG-109 a
08/252
|
08/362
|
09/1482
|
|
A/HK/1073/99 (G1 lineage)
|
H9N2
|
Wild type
07/210
|
08/208
|
07/1462
10/2143
|
|
A/chicken/Hong Kong/G9/1997 (G9 lineage)
|
H9N2
|
NIBRG-91 a
08/108
|
08/228
|
08/2022
|
|
Wild type
12/130
|
|
|
A/mallard/England/727/2006
|
H2N3
|
NIBRG-107 a
08/248
|
08/268
|
12/2502
09/1003
|
|
A/Singapore/1/1957
|
H2N2
|
NIBRG-147 a, b
09/306
|
|
00/440
08/3562
|
|
A/swine/Iowa/15/30
|
H1N1
|
NIBRG-196 a
10/186
|
|
|
|
A/Lviv/N6/2009
|
H1N1pdm09
|
NIBRG-162 a
10/184
|
|
|
|
A/Shanghai/2/2013
|
H7N9
|
NIBRG-267 a
13/118
|
|
13/1802
13/1663
|
|
A/Anhui/1/2013
|
H7N9
|
NIBRG-268 a
13/120
|
|